Ifeanyi Ugwuadu, Lead Editor, Insurance magazine and www.iintelnews.com
Subjects of Interest
- Capital Market
- Financial Market
- Insurance
Vitalising community-based social health insurance in Nigeria 15 Mar 2019
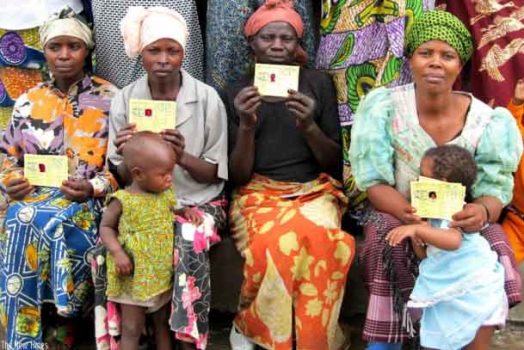
Mothers with children pose with their social health insurance 'Mutuelles de Sante' cards
The Nigerian healthcare system is weak and, thus, unable to deliver care adequately and efficiently to the vast majority of the population. While the formal sector has attained some level of coverage, healthcare provision in the informal sector is few and far between.
The National Health Insurance Scheme (NHIS) operates as a federal government health maintenance organisation (HMO) and a quasi-regulator of health insurance players in Nigeria. The dysfunctionalities in the system, including widespread graft, are already public knowledge. The system needs reform to facilitate access to affordable and insurance-driven healthcare system to Nigerians.
Under the current NHIS programme for public sector employees, the Federal Government pays the total bill, which is budgeted for annually. The funds are then transferred to NHIS as capitation payable to primary, secondary and tertiary hospitals. It is not clear if any deductions are made from the salaries of government employees to recoup the government’s premiums paid on behalf of the workers. In addition to the health insurance coverage that federal government employees receive, medical allowances are also paid to public sector workers.
Sadly, the current health insurance system does not address the need to expand access to healthcare. Rather, it caters more for the profiteering appetite of HMOs and insurance companies. The health care providers – that is, hospitals – and patients enrolled in the system bear the brunt of the weak system. In the end, hospitals often have to provide mediocre treatment to patients due to insufficient funding from the NHIS. Insurance companies and their HMOs are not prepared to take any risks.
Nigeria’s 198 million population is largely informal and rural, with patches of semi-urban communities. According to the National Population Commission's (NPC) 2008 Demographic and Health Survey (DHS), approximately 64 percent of the population lives in rural areas, and only 36 percent in urban areas. An understanding of the demographic profile is necessary for healthcare delivery and the provision of health insurance, which the low-income demographics can also afford.
There is a need for policymakers to revisit the Community-Based Social Health Insurance Programme (CBSHI) under the NHIS and promote the penetration of the scheme. This would require a critical re-evaluation of the blueprint and possibly incorporate some aspects of the Rwandan social health insurance model.
The Rwandan social health insurance programme, called Mutuelles de Santé was introduced in 1999 and achieved 91 percent subscription by 2005, according to the U.S.-based think tank, National Center for Biotechnology (NCBI). In contrast, the NHIS, which was established by the National Health Insurance Scheme Act, is 20 years old this year, and the scheme has achieved only about 5 percent enrolment.
The Mutuelles de Santé scheme is financed through insurance premiums contributed by both the government and individuals. Although subscription to the scheme is voluntary, it has been successful because it has provided improved medical care and protection of households against exorbitant medical spending. Though it is not without mismanagement scandals, the State has shown political will in dealing with issues of corruption.
To promote transparency and accountability, the country’s ministry of health had to be relieved of the responsibility of managing the scheme. The Rwanda Social Security Board (RSSB) was created to administer social security in the country. Apart from collecting all premiums under the health insurance and the Mutuelles de Santé, the RSSB also manages pension and occupational risks.
Suffice to say that as of 2014, Rwanda was the only country in Sub-Saharan Africa to achieve above 90 percent social health insurance coverage. To be able to move the needle in terms of improved health insurance coverage in Nigeria, there needs to be clear legislative and regulatory frameworks underpinning the social health insurance scheme. It needs to also be backed by adequate financial support and very clear enrolment requirements. It might also be necessary to break the scheme into three different tiers, with each tier having different jurisdictions – federal, state and local government areas (LGAs) – to improve enrolment.
The CBSHI should also be semi-independent from the NHIS, albeit regulated by the agency. A community-driven social health insurance scheme must necessarily be autonomous to promote trust and encourage more private sector participation.
On paper, the Nigerian CBSHI aims to improve access to health care services by eliminating or significantly reducing out-of-pocket payment for services. It also aims to improve quality of care by increasing both the amount and reliability of resources available for providers. Another objective is to improve efficiency in the allocation and use of available financial resources through improved accounting, financial management and utilization management tools, which in turn will help prevent fraud and abuse of the system. According to the blueprint on the implementation of the programme, it aims to make health services more equitable.
Stakeholders under the scheme include community members, programme managers – comprising of Boards of Trustees (BoTs) and technical facilitators. Other stakeholders are healthcare providers and the organized private sector. The programme managers are responsible for the day-to-day management of Mutual Health Associations (MHAs), which are groups that manage the community health insurance programmes.
There are a few successful community-based health insurance programmes in Nigeria, including the Hygeia Community Health Plan (HCHP). As of 2012, the scheme offered health insurance to about 177,500 people, including 67,500 in Lagos and 110,000 in Kwara State. Target groups under the scheme include market women and their families, farmers and their families, as well as staff of small businesses.
Another example of a CBSHI is in Anambra State where a government/ community healthcare co-financing scheme mobilises the community through a health committee. The scheme has enabled the refurbishment of the primary health care facilities, provision of drugs and employment of community members. The community members who enrol pay premiums of N50 per month for each child and N100 per month for each adult.
There are areas in which policymakers can optimise the present system. First, the government must determine a timeline to stop wholesale payment of medical bills with taxpayers’ money on behalf of and for its employees. The current system is neither equitable nor sustainable. If the NHIS is an insurance scheme, then everybody needs to pay.
A review of the legislative and regulatory frameworks for NHIS should include simply making the agency a regulator to govern health insurance schemes in the country. As the regulator, NHIS will also set standards for health care providers. The responsibility of management of funds should be transferred to the Board of the CBSHI that will be constituted.
Recognising the fact that any effort to deliver universal health coverage in the country must factor implementation and uptake of social health insurance in the informal sector, structures should be established to improve medical care for the low-income demographics, who would also be required to pay premiums, however little the amount each person or household can afford. Furthermore, the health care system in Nigeria needs to be redesigned for insurance-based health care delivery.
Despite the existence of the NHIS, out-of-pocket payments still characterise the bulk of transactions at health centres. Therefore, even in the context of the social health insurance, everyone will pay premiums. And on its part, the government will need to increase its investment in the sector as a matter of its social contract with the people.
Under the CBSHI blueprint, doctors and hospitals should play a dual role of being providers and also participating as programme managers in the community. This is because of the important role doctors, nurses, pharmacists and chemists play in most communities. Their inclusion as programme managers would boost trust and encourage more community members to enrol.
Latest Blogs By Ifeanyi Ugwuadu
- Nigerian regulators need to collaborate on financial inclusion
- Vitalising community-based social health insurance in Nigeria
- NAICOM needs to shed its toga as insurers' undertaker
- Improving business environment better than enforcing compulsory insurance
- How risk management tools can mobilise investment into Nigeria