The insidious threat of drug-resistant disease

Feature Highlight
Absent greater incentives, the development of new antimicrobial drugs will remain limited.
Forecast
- Absent greater incentives, the development of new antimicrobial drugs will remain limited.
- Rising global demand for meat and poultry will make it more difficult for governments to restrict the use of antimicrobial drugs in agriculture, especially in poorer countries.
- Different national interests will make it tough to achieve the international cooperation needed to combat the growing resistance to antimicrobial drugs.
Analysis
When Alexander Fleming discovered penicillin in 1928, he ushered in a new era of medicine: the age of antibiotics. Infections that had once been fatal could now be treated with relatively simple cures. In the decades that followed, penicillin became just one of many antimicrobial drugs that enabled humans and animals to live longer, more productive lives. The proliferation of those drugs seemed to have few, if any, downsides.
But over the years, we have gotten into the habit — as so often with other resources, including fish and fresh water — of overusing and misusing antimicrobial medicines. Doctors turned to them to treat illnesses, including viral infections, where antibiotics would not actually help. In time, microbes were able to build a resistance to the antibiotics deployed against them.
Now, that resistance poses a significant threat to the health of people and economies around the world. Global leaders gathered to address the growing danger at the U.N. General Assembly on Sept. 21. Though notable for the prominence of the forum hosting it, the meeting will probably yield few real solutions. An overwhelming number of economic and regulatory hurdles will make concerted international action on combating drug resistance as difficult to achieve as international action on climate change. Nations simply have more pressing priorities that will likely take precedence until an epidemic breaks out — one with economic consequences serious enough to spur the investment and cooperation needed to truly make a difference.
Unresponsive to Treatment
Microbes often mutate as they reproduce, providing a window for strains to develop a resistance to drugs. These random mutations, along with the surrounding environment, work together to determine a pathogen's evolution. How antimicrobial resistance builds in the future will therefore depend in part on the location of particular diseases and the agents being used to treat them. Different types of drugs target pathogens in different ways, determining the type of mutation that would best fend off the medicines' attacks. Moreover, some diseases become drug-resistant more quickly than others, which can make it difficult to pinpoint where they will next take root. So far, Russia and Central Asia have become hot spots for a drug-resistant strain of tuberculosis, while India has seen drug-resistant E. coli and salmonella emerge with a vengeance.
The overuse of antimicrobial drugs can speed up the natural process of building resistance. Studies have shown that roughly one-third of U.S. antibiotic prescriptions are unnecessary. Approximately the same share of antibiotics consumed in Southern and Eastern Europe are taken without a prescription. At the same time, nearly two-thirds of the antimicrobial drugs used in Africa are considered substandard, thanks in large part to the sale of counterfeit medications. Each of these issues, along with drug precursors and untreated medical waste disposal, can help diseases become resistant more quickly than they otherwise would.
Improving citizens' knowledge of, and government communication about, antibiotics will be critical to ensuring their more effective use. That said, as we have seen with vaccination campaigns, the reality on the ground will shape the success of these efforts. In the meantime, scientists must continue to craft new approaches to combating these diseases — an area that has largely lagged over the past few decades. Since the 1980s, the number of new antibiotics has sharply dropped off. Antibiotics are not highly profitable or attractive pursuits for most pharmaceutical companies. Though some promising discoveries have been made in recent years, the enormous costs associated with the creation of new drugs will likely hamper further progress. To effectively combat many of the world's ever-evolving diseases, that will need to change.
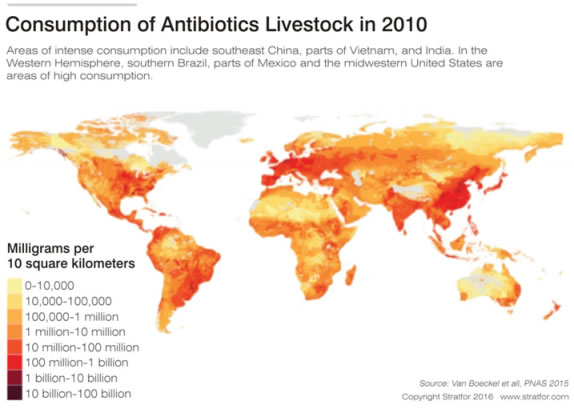
An Acute Problem in Agriculture
Despite the attention that has been paid to humans' reliance on antibiotics, the agricultural industry's use of the drugs may be more important to tamp down on in any campaign against drug resistance. By volume, 70 percent of the antibiotics approved for use in humans in the United States are used to treat livestock. And it is easy to see why: Studies show that a reduction in animal illness corresponds to a decline in human illness as well. The use of antimicrobial drugs in livestock can also promote animal growth and prevent or treat outbreaks among herds and flocks. For producers who are struggling to meet rising global demand for meat and poultry, boosting output is of chief concern. Though some countries, particularly in Europe, have banned the use of antimicrobial drugs to encourage livestock growth, no proven alternative has emerged to take their place in the industry.
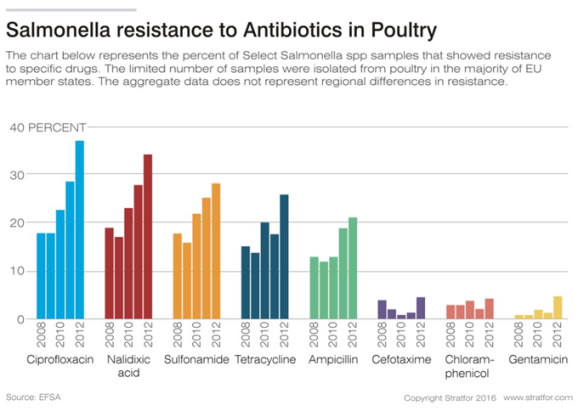
Considering how widely antibiotics are already being used, reining in their role in agriculture will be difficult to do without greater government surveillance and coordination. Though it is impossible to pinpoint exactly how much the agricultural sector contributes to the mounting resistance to antimicrobial drugs, the gains in production it makes from antimicrobial use must be balanced against any risk it creates. But the short-term losses in output that producers might experience if they abandoned antibiotics make it unlikely that the sector will change much of its own volition. A substantial shift would probably come only in response to a massive change in policy — something that, given the power of the agricultural sector in many countries, seems fairly unlikely.
Estimates that 10 million lives could be lost to drug-resistant disease each year by 2050 certainly grab headlines, but the potential economic ramifications are causing even greater concern among global leaders. Recent studies suggest that by 2030, antimicrobial resistance will cost the world more than $1 trillion per year. A large U.N.-led report shows that, depending on how widespread drug-resistant pathogens become, gross domestic products around the world could take a hit of between 1.1 and 3.6 percent by 2050. Of those states, low- to medium-income countries would experience the biggest blows to their GDPs. Others predict that the loss in global production could reach as high as $100 trillion.
The United Nations has proposed a plan to solve these problems that, if allowed to proceed, could go a long way in preventing such staggering losses. It calls, however, for improving surveillance, global coordination, research, health care and living standards in the developing world – all of which could cost, according to the United Nations, as much as $9 billion each year.
Ignoring the Signs
In today's globalized world, quashing superbugs requires the buy-in of every nation. But the U.N. proposal, though well intentioned, is unlikely to get it. In spite of the international resources that have been devoted to epidemics in recent years – Ebola and the Zika virus, to name a few – the problem of antimicrobial resistance is more chronic than acute. As with climate change, its economic symptoms are slow to manifest, and there are rarely immediate consequences for countries that fail to take action. Mobilizing a global effort to combat it will thus be equally hard.
In the short term, profit margins and rising demand will limit livestock producers' willingness to comply with any restrictions on the use of antimicrobial drugs that may be put in place. Meanwhile, the countries that are expected to be hit hardest by drug-resistant disease – those with low incomes – will have difficulty making the much-needed improvements in health care standards, sanitation and vaccination levels that would boost their chances of success.
There is, however, one scenario that could propel the global cooperation against drug resistance forward. Should a drug-resistant pathogen spark an acute, far-reaching epidemic, the international community would likely step up its efforts in response. Until then, the road to combating diseases' resistance to antimicrobial drugs will continue to be slow and arduous.
“The Insidious Threat of Drug-Resistant Disease” is republished with the permission of Stratfor and under content confederation between Financial Nigeria and Stratfor.
Other Features
-
At 50, Olajide Olutuyi vows to intensify focus on social impact
Like Canadian Frank Stronach utilised his Canadian nationality to leverage opportunities in his home country of ...
-
Reflection on ECOWAS Parliament, expectations for the 6th Legislature
The 6th ECOWAS Legislature must sustain the initiated dialogue and sensitisation effort for the Direct Universal ...
-
The $3bn private credit opportunity in Africa
In 2021/2022, domestic credit to the private sector as a percentage of GDP stood at less than 36% in sub-Saharan ...
-
Tinubunomics: Is the tail wagging the dog?
Why long-term vision should drive policy actions in the short term to achieve a sustainable Nigerian economic ...
-
Living in fear and want
Nigerians are being battered by security and economic headwinds. What can be done about it?
-
Analysis of the key provisions of the NERC Multi-Year Tariff Order ...
With the MYTO 2024, we can infer that the Nigerian Electricity Supply Industry is at a turning point with the ...
-
Volcanic explosion of an uncommon agenda for development
Olisa Agbakoba advises the 10th National Assembly on how it can deliver on a transformative legislative agenda for ...
-
Nigeria and the world in 2024
Will it get better or worse for the world that has settled for crises?
-
The Movers and Shakers of Nigeria 2023
This special publication profiles 25 people and institutions based on their societal or industry impact in 2023.
Most Popular News
- IFC, partners back Indorama in Nigeria with $1.25 billion for fertiliser export
- Ali Pate to deliver keynote speech at NDFF 2024 Conference
- Univercells signs MoU with FG on biopharmaceutical development in Nigeria
- CBN increases capital requirements of banks, gives 24 months for compliance
- CBN settles backlog of foreign exchange obligations
- Nasdaq Dubai welcomes $600m sukuk listing by Islamic Development Bank